
Welcome to Amanda's NICU Education




Hi! My name is Amanda. I'm a NICU nurse, Clinical Nurse Specialist, NICU Educator... basically your NICU BFF. If you want to talk NICU, I'm here for you! I love everything about NICU nursing and I'm eager to learn and share my knowledge with all my NICU friends.
I have been a NICU nurse since 2009 I am currently a Clinical Nurse Specialist in a Level IV NICU in Los Angeles.
I am passionate about educating the next generation of NICU nurses. I share my knowledge through platforms such as Instagram and Facebook and am excited to have you here on my website!
Click on the button below to sign up for my newsletter filled with NICU education and tips for all experience levels.

Not very many people love taking tests but as a self-acclaimed "forever student" who has taken (and passed) five different certification exams I am no longer afraid of tests! "Way to brag", you might be thinking but I want to help YOU pass your certification exam too!
Introducing Amanda's RNC-NIC Success digital course - your ultimate study companion!
Gain unlimited, on-demand access for life, ensuring you're primed to ace your certification exam.
I'm here to help you succeed and I can't wait for you to share with me that you PASSED the RNC-NIC EXAM!!!









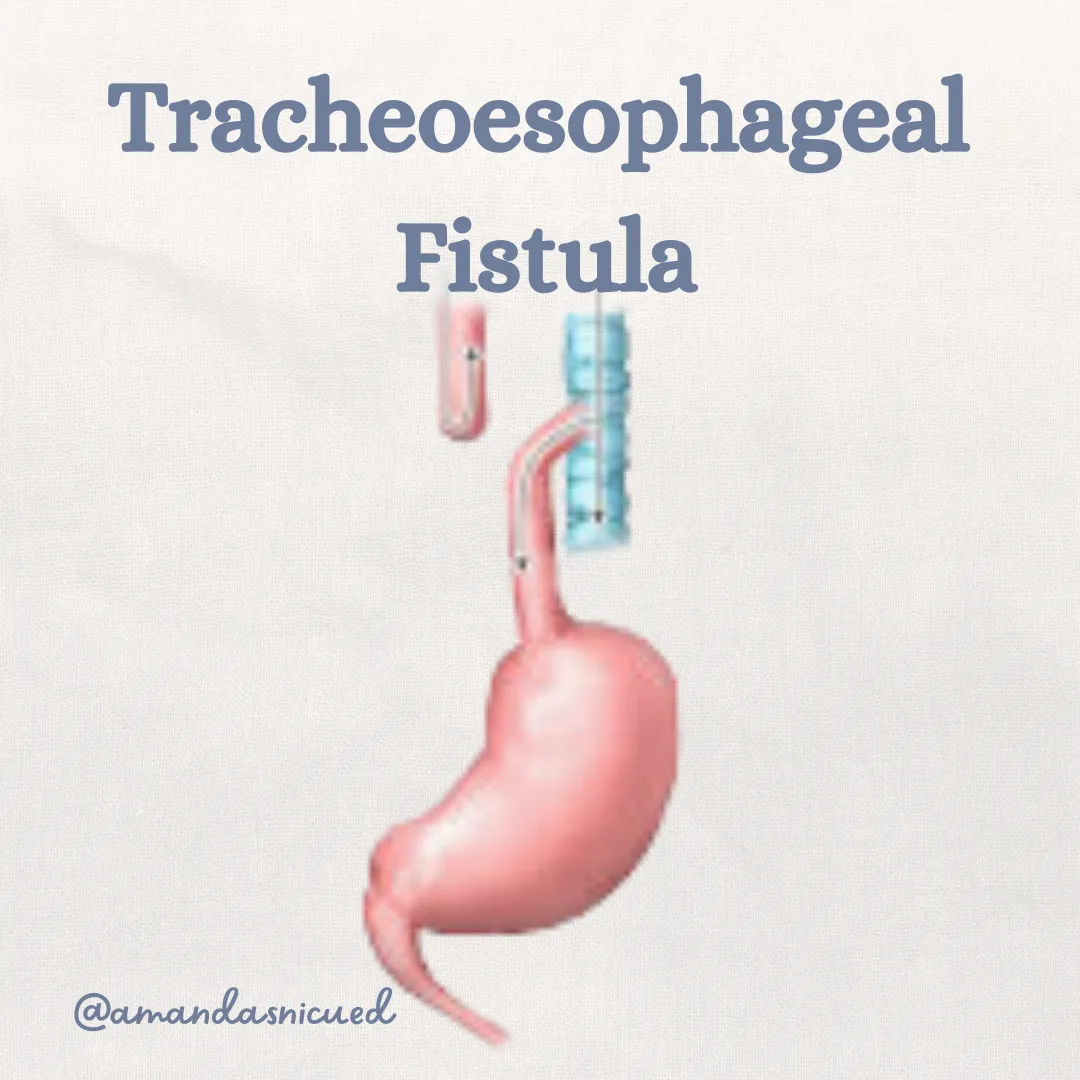
TEF
Esophageal Atresia & Tracheoesophageal Fistula
Have you ever noticed how certain conditions seem to show up repeatedly, almost like they come in threes? Lately, I’ve been seeing a lot of TEF cases around me. It feels like a sign from the universe that it’s time for us to review TEF together!
Embryology:
Early in embryologic development the trachea and esophagus start out as one tube. As development progresses, there is septation, separating the trachea and esophagus. Tracheoesophageal fistula (TEF) results from incomplete separation during the 4th to 6th weeks of embryonic development. Esophageal Atresia (EA) can occur on its own, or alongside TEF. The incidence of TEF is about 1-2 in every 3500 live births. Most cases occur sporadically, however there are some recognized genetic associations. EA/TEF has been reported in patients with Pierre Robin sequence, DiGeorge (22q11.2 deletion), and Trisomies 13, 18, or 21.
Types of Defects
TEF and EA are categorized into five types, with Type C (esophageal atresia with a distal fistula) being the most common:
Type A: Esophageal atresia without a fistula.
Type B: Esophageal atresia with a proximal fistula.
Type C: Esophageal atresia with a distal fistula (most common).
Type D: Esophageal atresia with both proximal and distal fistulas.
Type E: Isolated TEF without atresia.

van Lennep, 2019
Signs and Symptoms
The presentation will depend on the specific type of EA/TEF, as they are all anatomically different. When we are caring for a newborn we may suspect EA/TEF if we see the following signs:
Maternal history of polyhydramnios (can be a sign of a proximal GI obstruction)
Excessive drooling/salivation
Feeding intolerance: Cyanosis or choking with feeds
Respiratory distress
Inability to pass an orogastric (OG) tube or an OG tube that coils and comes back out the mouth
On X-Ray you may see the OG tube stops or coils above the carina (often T2-3)
Abdominal distention (in cases with a distal fistula).
Diagnosis
The diagnosis is made through imagining. Visualization of the OG tube in the proximal esophagus and air in the stomach/bowel is indicative of a fistula present (otherwise how would the air make its way down to the stomach?). Contrast studies (upper GI) can be done to provide more clarification of the anatomy.
Some types of TEF, such as the H-type, are more difficult to diagnose as they have a more subtle presentation. These patients may present with feeding difficulty and history of pneumonia (due to aspiration via the fistula). The H-type fistula can be difficult to confirm on imaging and may require rigid bronchoscopy.

Dingeldein, 2025
Treatment
Surgical repair: Definitive treatment involves closure of the fistula and reanastomosis of the esophageal segments.
Staged procedures: Some infants, (preterm, critically ill neonates, or those with too long of a gap between the esophageal pouch and the stomach) may require staged approaches with gastrostomy placement first.
Nursing Considerations
Pre-operative care of the baby with EA/TEF involves ensuring a large bore OG tube is inserted into the esophageal pouch and set to low continuous suction. Managing secretions is important to prevent aspiration. Additionally the head of bed is elevated and the baby may be placed prone to reduce reflux through the fistula. Parenteral Nutrition will be provided until it is safe to feel the baby enterally.
When caring for babies with EA/TEF, nurses should be aware of the constellation of defects known as VACTERL association. VACTERL association, a variable sequence of anomalies affecting the Vertebrae, Anus, Cardiac system, Trachea, Esophagus, Renal (urinary tract), and Limbs. Evaluation for other anomalies (e.g. Echocardiogram) will be performed.
Post-operative nursing care always involves pain management, infection prevention, and supporting the family. In cases of EA/TEF, there are some specific considerations nurses must keep in mind.
Do NOT deep suction or place a new OG tube. This can cause injury to the anastomosis site
Sometimes babies may return from surgery with a surgically placed replogle/OG tube. It is imperative that this tube stays in place. If it becomes dislodged the surgical team must be notified.
A chest tube may be in place to control anatomic air leak from the surgery. When caring for a baby with a chest tube frequently monitor:
Tube patency and signs of air leak
Drainage amount, color, and consistency
Signs of infection or dislodgement
Ensure emergency supplies for chest tubes are at the bedside
An esophagram will be performed to assess for a leak at the anastomosis site approximately 5-7 days after repair. Anastomotic leaks, strictures, and/or esophageal dysmotility are a few complications that can be seen after EA/TEF repair. If a leak is present treatment involves chest tube drainage, parenteral nutrition, and patiently waiting. Most leaks resolve on their own with time. Esophageal strictures may require dilation to maintain esophageal patency.
Family Support
Caring for an infant with TEF and EA is overwhelming for families. We can offer support by:
Providing clear explanations about the defect and the treatment plan.
Encouraging their involvement in non-medical care, such as skin-to-skin contact or containment.
Does your NICU allow holding of patients with chest tubes?
Connecting them with support groups or resources specific to congenital anomalies.

TEF and EA require a multidisciplinary approach involving skilled NICU nursing care, effective communication, and family-centered support. Your attention to detail and compassionate care make a lasting difference for these vulnerable babies and their families.
Let’s continue to provide exceptional care and education for our NICU families. Thank you for all you do!
Warm regards,
Amanda
Missed my other newsletters? Click here to read them!
Let's Study Together! Join my Certification Course
Reference:
Dingeldein, M. (2025) Selected Gastrointestinal Anomalies in the Neonate in Fanaroff and Martin’s Perinatal Medicine (12th Ed). Elsevier
Gallagher, M., Pacetti, A., Lovvorn, H., Carter, B. (2021). Neonatal Surgery in Merenstein & Gardner’s Handbook of Neonatal Intensive Care(9th Ed). Elsevier
van Lennep, M., Singendonk, M. M. J., Dall'Oglio, L., Gottrand, F., Krishnan, U., Terheggen-Lagro, S. W. J., Omari, T. I., Benninga, M. A., & van Wijk, M. P. (2019). Oesophageal atresia. Nature reviews. Disease primers, 5(1), 26.

December 2023 Certification Review Webinar
NICU Certification Review



Ready to kickstart your journey to becoming a certified NICU nurse?
Look no further!
Grab my FREE E-Book packed with essential study and test-taking strategies for the RNC-NIC.
In the E-Book I give you the resources you need including the link to access the candidate guide, several types of books to study from, some of my favorite strategies, an outline of the content you should review, and a blank calendar for you to make your study plan!
Frequently Asked Questions About the RNC-NIC exam

What is the RNC-NIC?
The RNC-NIC is a competency-based exam that tests the specialty knowledge of nurses in the United States & Canada who care for critically ill newborns and their families.
The RNC-NICU is a nationally recognized certification that recognizes the registered nurse for their specialty knowledge and skill.

Who can take the RNC-NIC exam?
Nurses can take this exam after a minimum of two years experience in the NICU caring for critically ill newborns and their families.

Which books should I use?
I'm glad you asked! There are many excellent books to help you prepare for the RNC-NIC, I gathered ande describe each of them for you in my FREE e-book.
Is there a course to help me study?
Yes! Many hospitals host their own certification course and there are a few online courses. See my RNC-NIC test taking tips E Book for more information
What happens if I don't pass the exam?
If you don't pass the exam on your first try you can try again after 90 days. You will have to reapply after 90 days and pay a retest fee. There is no limit to the number of times you can take the exam (however a candidate can only sit for the exam twice per year).

Can I make more money if I take the RNC-NIC exam and get certified?
Yes! Many hospitals provide a raise or a bonus for nurses with specialty certifications. Hospitals also typically hire at a higher base salary when nurses have a certification.

Find me @amandasnicued on these channels or Email me
hey nurses don't miss out
© Copyright 2024. AmandasNICUEd. All rights reserved. | Terms & Conditions | Privacy Policy Contact: [email protected]

