
Welcome to Amanda's NICU Education




Hi! My name is Amanda. I'm a NICU nurse, Clinical Nurse Specialist, NICU Educator... basically your NICU BFF. If you want to talk NICU, I'm here for you! I love everything about NICU nursing and I'm eager to learn and share my knowledge with all my NICU friends.
I have been a NICU nurse since 2009 I am currently a Clinical Nurse Specialist in a Level IV NICU in Los Angeles.
I am passionate about educating the next generation of NICU nurses. I share my knowledge through platforms such as Instagram and Facebook and am excited to have you here on my website!
Click on the button below to sign up for my newsletter filled with NICU education and tips for all experience levels.

Not very many people love taking tests but as a self-acclaimed "forever student" who has taken (and passed) five different certification exams I am no longer afraid of tests! "Way to brag", you might be thinking but I want to help YOU pass your certification exam too!
Introducing Amanda's RNC-NIC Success digital course - your ultimate study companion!
Gain unlimited, on-demand access for life, ensuring you're primed to ace your certification exam.
I'm here to help you succeed and I can't wait for you to share with me that you PASSED the RNC-NIC EXAM!!!









Intraventricular Hemorrhage
Intraventricular Hemorrhage
This month, let’s review a common morbidity among premature babies that we all actively work to prevent: intraventricular hemorrhage (IVH).

What is IVH?
Intraventricular hemorrhage occurs due to bleeding in the brain, typically originating in the fragile germinal matrix and extending into the ventricles. IVH is a significant risk factor for brain injury and subsequent neurodevelopmental impairment in preterm infants. This is an essential topic for NICU nurses to stay informed about the latest evidence-based care, ensuring the best outcomes for their patients.
Who is Most at Risk of IVH?
Premature infants born at less than 32 weeks of gestation are at the highest risk for IVH. The more premature the infant, the greater the risk. Extremely low birth weight babies (<750g) have a 10-fold higher likelihood of severe IVH compared to infants weighing >1250g at birth.
Additional risk factors include:
Chorioamnionitis
Perinatal hypoxic-ischemic events
Use of sodium bicarbonate
Significant delivery room resuscitation
Neonatal transport
How Does IVH Happen?
The germinal matrix, located just below the ventricles, is a highly vascular structure involved in angiogenesis (blood vessel development) and producing neuronal and glial progenitors. This matrix gradually decreases in size and typically involutes (disappears) by 34-36 weeks of gestation. Therefore in premature infants less than 32 weeks, the germinal matrix remains present and is extremely fragile and at risk for bleeding. The blood vessels within the germinal matrix have a “U-turn”, making it extremely vulnerable to fluctuations in blood flow and pressure.
IVH often occurs due to increased venous pressure or cerebral blood flow fluctuations. Unlike term infants, the preterm brain is “pressure-passive” and lacks the ability to autoregulate blood pressure effectively. This makes it particularly sensitive to:
Hypotension followed by reperfusion
Isolated hypertension or increased cerebral blood flow caused by events like seizures, intubation, suctioning, or surfactant administration
The highest risk of IVH is within the first three days of life, with approximately half of neonatal hemorrhages occurring within the first six hours. Small nuances in care, such as rapid bolus infusion or lifting the hips during a diaper change, can influence IVH risk, highlighting the critical role of NICU nurses in prevention.
Luo, 2019
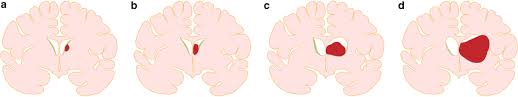
Grades of IVH
The severity of IVH is categorized into four grades based on the extent of hemorrhage:
Grade 1: Germinal matrix hemorrhage (<10% of ventricular volume).
Grade 2: Hemorrhage involving 10-50% of the ventricular volume.
Grade 3: Hemorrhage involving >50% of ventricular volume, often causing lateral ventricle distension.
Periventricular Hemorrhagic Infarction: Echodensity in the periventricular region.
Historically, “Grade IV” referred to hemorrhage extending from the ventricle into the parenchyma. However, experts now view this as a distinct process (parenchymal venous infarction) rather than an extension of IVH.
IVH may also disrupt cerebellar development due to its high population of progenitor cells, which are vulnerable to blood products. Advanced MRI techniques have identified primary hemorrhages in the cerebellar germinal matrix.
Signs of IVH
Clinical signs of IVH vary widely, from asymptomatic presentations to sudden, severe deterioration. Symptoms may include:
Apnea
Tense, full fontanelle
Drop in hematocrit
Widened sutures
Increasing head circumference
Seizures
Posturing
Hypotension
Diagnosis is made through routine cranial ultrasounds.
Management of IVH
Management of IVH is primarily supportive and includes:
Serial ultrasounds to monitor for complications (e.g., post-hemorrhagic ventricular dilation).
Blood transfusions for significant drops in hemoglobin or hematocrit.
EEG or aEEG monitoring to detect seizure activity.
Surgical interventions, such as ventricular reservoirs or ventriculoperitoneal (VP) shunts, in cases of posthemorrhagic hydrocephalus.
Outcomes of IVH
Grades 1 and 2: These typically resolve over time, though inflammation and neurotoxic effects may disrupt white matter, impair myelination, and lead to cortical and thalamic dysmaturation. Long-term sequelae remain uncertain, emphasizing the need for follow-up care.
Grade 3: Associated with increased risk of periventricular white matter injury. Neurodevelopmental outcomes may depend on the timing of interventions for posthemorrhagic ventricular dilation.
Periventricular Hemorrhagic Infarction: A significant predictor of neurodevelopmental impairment, commonly causing unilateral spastic hemiplegia (cerebral palsy) contralateral to the hemorrhage.
How Can We Prevent IVH?
Since IVH treatment is primarily supportive, prevention is critical. Preventative strategies include:
Prenatal care: Maternal steroids and management of chorioamnionitis.
Antenatal interventions: Delayed cord clamping, ensuring thermoregulation/preventing hypothermia, and experienced resuscitation teams.
NICU care: Measures to reduce cerebral blood flow fluctuations and stress, such as gentle two-person care, positive sensory experiences, ensuring that boluses are given slowly and the legs/hips are never lifted above the head.
Let’s review the evidence for a few specific interventions:
Head positioning: Evidence is mixed. Some studies suggest elevated head positioning may benefit survival and reduce severe IVH, a Cochrane review in 2020 found there is no strong evidence that a specific head position significantly reduces IVH.
Ventilation management: Complications of over or under ventilation result in fluctuations in cerebral blood flow and elevated central venous pressure.
Hypocarbia is associated with hypotension and increased risk of IVH and white matter injury.
Hypercardia results in vasodilation leading to increased cerebral blood flow.
Delivering high tidal volumes (>6mL/kg) during the positive pressure ventilation in the delivery room was shown to increase the rate of severe IVH.
Avoiding harmful medications: Sodium bicarbonate is associated with increased IVH risk, potentially due to hyperosmolarity, sodium fluctuations, and hypernatremia.
Prophylactic indomethacin: Some centers administer indomethacin prophylactically to reduce IVH. Studies have shown prophylactic indomethacin reduces severe IVH and the incidence of symptomatic PDA but did not seem to impact long term outcomes.
One study examined a cohort of NICUs over a ten year period and found indomethacin prophylaxis decreased over the ten year period among most NICUs in the cohort with no change in IVH.
NIRS Monitoring: Some NICUs utilize Near Infrared Spectroscopy during the first 72 hours of life. NIRS provides non-invasive measurements of changes in cerebral perfusion and oxygenation. It has the potential of providing real time information on cerebral blood flow.
A Phase 3 randomized control trial conducted at 70 sites looking at 1601 infants did not find a lower incidence of death or severe brain injury at 36 weeks in extremely preterm infants guided by NIRS monitoring for the first 72 hours compared to usual care.

Does your NICU have an IVH prevention bundle? What is included? Email me and let me know if you do something I didn't mention. I'd love to hear about your practices in your NICU and how you are working with your team to prevent IVH!
Stay curious,
Amanda
Missed my other newsletters? Click here to read them!
Let's Study Together! Join my Certification Course
References:
Riddle, A., Miller, S., & Back, S. (2024). Brain injury in the preterm infant in AVery’s Diseases of the Newborn. Elsevier
Cizmeci, M & Vries, L. (2025). Intracranial Hemorrhage and Stroke in the Neonate in Fanaroff and Martin’s Neonatal Perinatal Medicine (12th Ed). Elsevier
Kolnik, S. E., Upadhyay, K., Wood, T. R., Juul, S. E., & Valentine, G. C. (2023). Reducing Severe Intraventricular Hemorrhage in Preterm Infants With Improved Care Bundle Adherence. Pediatrics, 152(3), e2021056104.
Garvey, A. A., Walsh, B. H., & Inder, T. E. (2022). Pathogenesis and prevention of intraventricular hemorrhage. Seminars in perinatology, 46(5), 151592.
Matlock D. N., Jr (2019). Does an elevated midline head position prevent periventricular-intraventricular haemorrhage in extremely low birth weight neonates?. Acta paediatrica (Oslo, Norway : 1992), 108(10), 1925.
Romantsik, O., Calevo, M. G., & Bruschettini, M. (2020). Head midline position for preventing the occurrence or extension of germinal matrix-intraventricular haemorrhage in preterm infants. The Cochrane database of systematic reviews, 7(7), CD012362.
Al-Matary, A., Abu Shaheen, A., & Abozaid, S. (2022). Use of Prophylactic Indomethacin in Preterm Infants: A Systematic Review and Meta-Analysis. Frontiers in pediatrics, 10, 760029.
Curtis, S. F., Cotten, C. M., Laughon, M., Younge, N., Peterson, J., Clark, R. H., & Greenberg, R. G. (2024). Indomethacin Prophylaxis in Preterm Infants: Changes over Time. American journal of perinatology, 41(S 01), e680–e688.
Hansen, M. L., Pellicer, A., Hyttel-Sørensen, S., Ergenekon, E., Szczapa, T., Hagmann, C., Naulaers, G., Mintzer, J., Fumagalli, M., Dimitriou, G., Dempsey, E., Tkaczyk, J., Cheng, G., Fredly, S., Heuchan, A. M., Pichler, G., Fuchs, H., Nesargi, S., Hahn, G. H., Piris-Borregas, S., … Greisen, G. (2023). Cerebral Oximetry Monitoring in Extremely Preterm Infants. The New England journal of medicine, 388(16), 1501–1511.
Luo, J., Luo, Y., Zeng, H., Reis, C., & Chen, S. (2019). Research Advances of Germinal Matrix Hemorrhage: An Update Review. Cellular and molecular neurobiology, 39(1), 1–10. https://doi.org/10.1007/s10571-018-0630-5

December 2023 Certification Review Webinar
NICU Certification Review


Ready to kickstart your journey to becoming a certified NICU nurse?
Look no further!
Grab my FREE E-Book packed with essential study and test-taking strategies for the RNC-NIC.
In the E-Book I give you the resources you need including the link to access the candidate guide, several types of books to study from, some of my favorite strategies, an outline of the content you should review, and a blank calendar for you to make your study plan!
Frequently Asked Questions About the RNC-NIC exam

What is the RNC-NIC?
The RNC-NIC is a competency-based exam that tests the specialty knowledge of nurses in the United States & Canada who care for critically ill newborns and their families.
The RNC-NICU is a nationally recognized certification that recognizes the registered nurse for their specialty knowledge and skill.

Who can take the RNC-NIC exam?
Nurses can take this exam after a minimum of two years experience in the NICU caring for critically ill newborns and their families.

Which books should I use?
I'm glad you asked! There are many excellent books to help you prepare for the RNC-NIC, I gathered ande describe each of them for you in my FREE e-book.
Is there a course to help me study?
Yes! Many hospitals host their own certification course and there are a few online courses. See my RNC-NIC test taking tips E Book for more information
What happens if I don't pass the exam?
If you don't pass the exam on your first try you can try again after 90 days. You will have to reapply after 90 days and pay a retest fee. There is no limit to the number of times you can take the exam (however a candidate can only sit for the exam twice per year).

Can I make more money if I take the RNC-NIC exam and get certified?
Yes! Many hospitals provide a raise or a bonus for nurses with specialty certifications. Hospitals also typically hire at a higher base salary when nurses have a certification.

Find me @amandasnicued on these channels or Email me
hey nurses don't miss out
© Copyright 2024. AmandasNICUEd. All rights reserved. | Terms & Conditions | Privacy Policy Contact: [email protected]

